- Advertise
- About OncLive
- Editorial Board
- MJH Life Sciences brands
- Contact Us
- Privacy
- Terms & Conditions
- Do Not Sell My Information
2 Clarke Drive
Suite 100
Cranbury, NJ 08512
© 2025 MJH Life Sciences™ and OncLive - Clinical Oncology News, Cancer Expert Insights. All rights reserved.
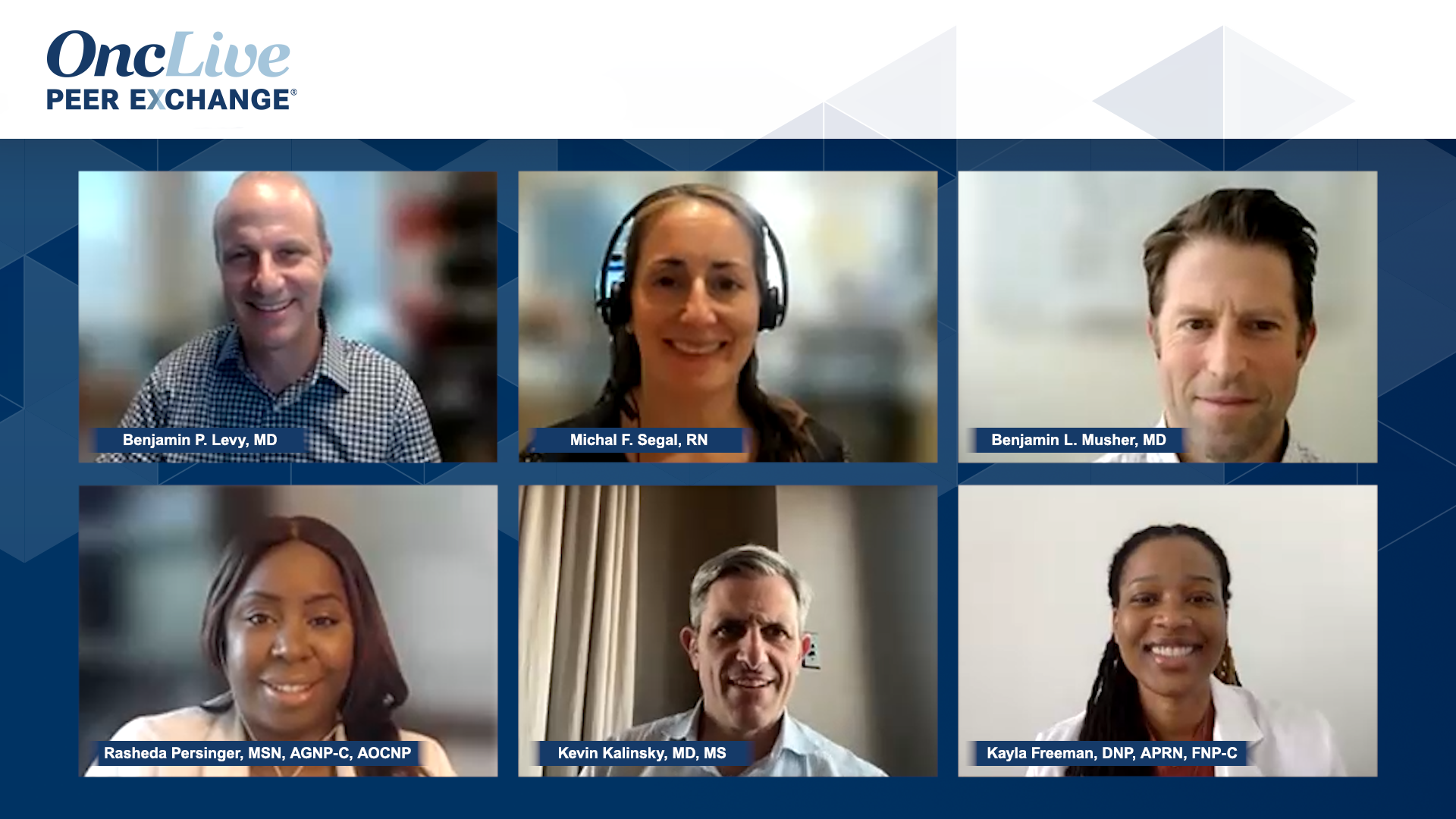
Managing T-DXd Toxicities in Gastric Cancer
Insights on managing antibody-drug conjugate toxicities for patients with gastric cancer.
Sponsored in part by Daiichi Sankyo. Content independently developed by OncLive®.
Transcript:
Benjamin P. Levy, MD: Michal [F. Segal, RN], what has been your experience at Memorial [Sloan Kettering Cancer Center in New York, New York] with this drug and gastric [cancer]? How do you get patients through it and the toxicities that you may see? What has been your experience there?
Michal F. Segal, RN: Just to clarify, we do the starting dose of 6.4 mg/kg. We do have new studies or reopening studies where the new dose is going to be 5.4 mg/kg. But, we give the off-study trastuzumab deruxtecan [T-DXd] as a second-line therapy. The rationale is that it’s targeted therapy, whereas Ram-Taxel [ramucirumab and paclitaxel] we can always give later and is nontargeted. Usually, patients are agreeable to try something that’s not technically chemotherapy and the schedule is better. So we will do that second line. Toxicity wise, usually we will dose reduce after the first scan and if a patient has persistent nausea and fatigue; those were the biggest things we saw. Then in relation to giving all the antiemetics, a lot of them are constipated. So fatigue was pretty moderate, staying in bed all day, that is something we would dose reduce for. But toxicity wise, it is generally nice compared with other therapies. And then for the ILD [interstitial lung disease] pneumonitis, typically we’ll work that up according to the protocol that it was approved upon where it’s extremely stringent; if the patient has a cough, we’d get a chest x-ray or a CT or sometimes their scan will show some mild lung changes and the patient could be asymptomatic, but we’ll still air on the side of caution and maybe get a CT right away or PFTs [pulmonary function tests] But generally, it’s well tolerated. It’s every 3 weeks. So that’s nice. You don’t go home with a [5-fluorouracil] bottle. So there’s a lot of appealing things to it.
Benjamin P. Levy, MD: Yeah.
Benjamin L. Musher, MD: One thing I’ll add also: Remember, first-line therapy in gastric cancer is going to include oxaliplatin. Your second line is going to be your taxane. One of the common toxicities has been neuropathy.
Going from platinum into the taxane can be tough. And unlike colon cancer, we know that we can drop it after a few months. Even though that sort of makes sense, in gastric cancer, we don’t have those data. So giving people a break off that platinum and letting the neuropathy cool down is actually a great thing to do as well. It makes perfect sense in my opinion.
Benjamin P. Levy, MD: Yeah, [it is] remarkable to see the trajectory of these types of drugs in different tumor types. Rasheda, did you want to say something?
Rasheda Persinger, MSN, AGNP-C, AOCNP: Just a quick question. I’m just curious. With the higher dose in the GI [gastrointestinal] population, do you see a lot of ILD disease or no, not so much? Is that a common thing? Because I’m just thinking of the handful of patients, and granted, it’s just a handful of patients that we have and I know we’re in a lower dose. I don’t really see even those symptoms or concerns or a workup for ILD.
Benjamin L. Musher, MD: And you guys also have patients who already have lung disease, right?
Rasheda Persinger, MSN, AGNP-C, AOCNP: Right.
Benjamin L. Musher, MD: Right. Ours typically don’t. I’ve only seen 1, maybe 2 cases of it. I’ve only seen a couple of them. I don’t know. I don’t know how many you’ve seen, Michal. Or that I’m convinced had it.
Michal F. Segal, RN: It’s definitely a handful. It wasn’t some large amount that if we dose reduced, we saw different outcomes. I think maybe the reduction they’re doing to 5.4 mg/kg is just because it’s part of a clinical trial. I guess they’re trying to test efficacy with a dose that other diseases are using already. But no, I didn’t think the trial that we did with 6.4 mg/kg, the whole trial stayed at that dose. We neve…the trial didn’t modify or deviate frailty. I don’t think we saw a greater percentage of people at the higher dose.
Benjamin L. Musher, MD: I don’t do scans every 6 weeks. One thing I do is not only to ask people a lot of questions about their exercise tolerance. I just put the SAT [pulse oximeter that measures oxygen saturation] monitor on and walked them around the unit a couple of times. Because, you know, sometimes that’s the first thing people don’t notice, right? Which is that they’re desaturated with more exertion. So even at the slightest hint, a patient saying, “I can’t climb 2 or 3 flights of stairs like I used to.” I’ve got a pretty low threshold to do that; it’s cheap and it’s quick and I can do it right there in the clinic. Is there any validity to it? I have no idea. But it’s certainly cheaper and easier than a CT scan.
Benjamin P. Levy, MD: We love SAT monitors in our clinic. We need them for many different reasons because IO [immuno-oncology] therapies are so important.
Transcript is AI-generated and edited for clarity and readability.
Related Content: