- Advertise
- About OncLive
- Editorial Board
- MJH Life Sciences brands
- Contact Us
- Privacy
- Terms & Conditions
- Do Not Sell My Information
2 Clarke Drive
Suite 100
Cranbury, NJ 08512
© 2025 MJH Life Sciences™ and OncLive - Clinical Oncology News, Cancer Expert Insights. All rights reserved.
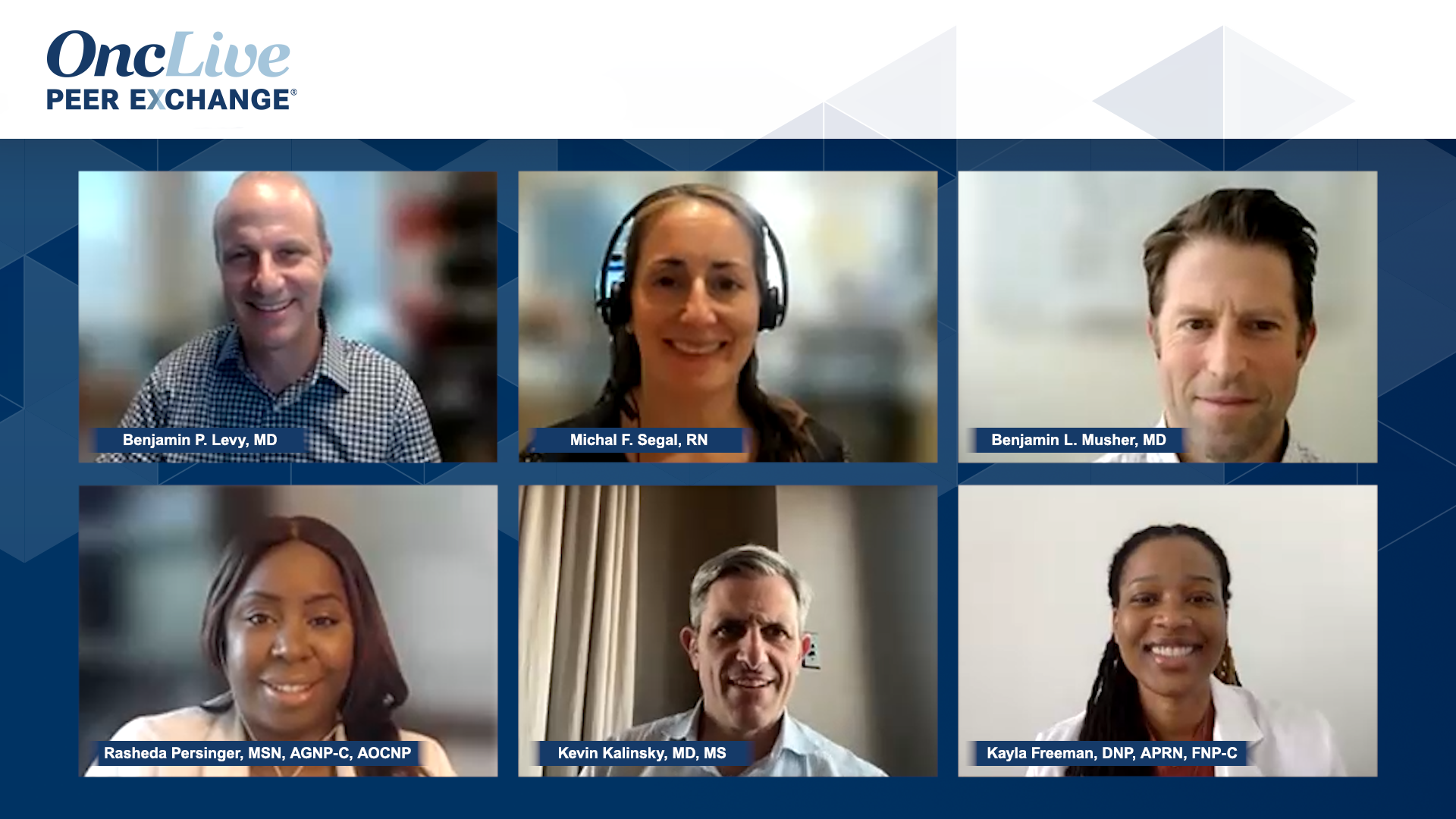
Biomarker Testing in Gastrointestinal and Lung Cancers
Comprehensive insights on biomarker testing practices for patients with lung or gastrointestinal cancers.
Sponsored in part by Daiichi Sankyo. Content independently developed by OncLive®.
Transcript:
Benjamin P. Levy, MD: I know, Michal and Ben, you’re at different institutions, but I want to tackle GI [gastrointestinal] here. Maybe I’ll start with Michal first. What does the patient journey look like for testing in the GI world, gastric and colorectal? I know you’ve got a lot to deal with, but what does that look like at [Memorial Sloan Kettering Cancer Center in New York, New York]? Then, Ben, we will go over to you and talk about what you’re testing for at [Baylor College of Medicine Dan L Duncan Comprehensive Cancer Center in Houston, Texas].
Michal F. Segal, RN: Patients come to us already diagnosed, so they’ll have outside pathology already done and then it’s a free-for-all in terms of how much information the outside institution provided the patient with. A lot of times there is usually a standard pathology and then an addendum will have all the biomarkers. So we look at MSI [microsatellite instability] PD-L1 [programmed death ligand-1], HER2 [human epidermal growth factor receptor 2], and EBV [Epstein-Barr virus]; there are a few for gastric and esophageal that we look for. So oftentimes a patient’s coming from outside. They’ll bring the report, they’ll bring some slides, and the report will say addendum pending and then the patient needs to, ideally, follow-up to get any addendums, but it’ll then fall on us to chase those results. In the meantime, we’ll try to get slides from their procedure and then do our own testing. But, sometimes, in the interest of time, we’ll get a new endoscopy just to get tissue in-house. Once it’s in-house, there are automatic biomarkers that are done with our pathology without us ordering them. So they’ll automatically do the ones that we want. Reflex is done if it’s hard to equivocal; they’re automatically reflex to FISH [fluorescence in situ hybridization]. The biggest barrier typically is getting addendums. If they’re even done, it’s extremely inconsistent. And then after that, it’s getting tissue, either our own or getting outside slides. That’s the race against time.
Benjamin P. Levy, MD: It’s a good point. And I want to touch on barriers when we finish here because I think lung has some. We all have major barriers. Tissue is precious and we often have a difficult time getting enough. Ben, what is your experience with testing for GI malignancies at Baylor, and how does it go down? How are patients ushered through that diagnostic paradigm before they get treated?
Benjamin L. Musher, MD: The tissue issue is always a big problem, and we’ve struggled a lot with this in conversation with our pathologists. How much of the tissue are we going to start using up for these individual stains vs getting everything to next-generation sequencing [NGS], which we did for everybody anyway? There are certain things that are going to change our management very quickly. The mismatch repair defense deficiency is huge because we’re using, obviously, checkpoint inhibitors up front and a lot of people now have PD-L1…I think that can play one way a little bit. The HER2 is important as well. So the way we do it, I see patients out there at our county hospital, which is a fully academic hospital, and our university hospital, and, thankfully, we have a contract with Tempus, so they will actually sequence all of our patients for free in the county hospital, and then insurance usually [does it] for nothing at our university. So that’s really nice. So we send everything to Tempus. We will do HER2 staining and then our staining for mismatched proteins up front. Everything else gets sent off. Sometimes tissue gets burned up, which is a problem. The nice thing about contracting with an outside place is if a patient comes in from the outside, we don’t have to get the tissue, we put the order in the EMR [electronic medical records], and Epic and then Tempus gets the tissue directly from the outside labs. So we don’t lose time that way, but we’re pretty much sequencing everybody for everything. And obviously, the staining has to be done separately with HER2. But you also pick up some unusual stuff. You’ll pick up, the anthrax and the ones you don’t expect to pick up. But, usually, it’s going to be about those biomarkers, MMR, PD-L1, and HER2.
Benjamin P. Levy, MD: I think Baylor’s 3 steps ahead of Hopkins [Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Washington, DC]. We are wrestling right now with this very concept—should we be doing third-party vendors and having, in some scenarios, an order set in Epic? We do in-house testing, but I don’t want to steal Rasheda’sthunder because she knows the journey for our patients a lot of times better than us. Rasheda, do you want to walk us through what we test for, how we test it, and what that journey looks like because you’ve been sort of the general for all of this, for lung cancer, not just here in DC, but for all of Hopkins.
Rasheda Persinger, MSN, AGNP-C, AOCNP: When it comes to the patient journey, I think the first thing you have to begin with is how they present to us. Are they being presented to us by our interventional pulmonology, or are they coming in for a second opinion? That determines their particular journey. We have a great working relationship with great communication and a really valuable interdisciplinary relationship with our pulmonary department. Therefore, Dr Andrew Lerner will more than likely send us a heads-up, “Hey, I got this sample. What testing needs to be done?” So the clock starts there. Unfortunately, we don’t have reflex, so it has to be ordered for each patient. For metastatic patients, the typical ones, we’re doing complete NGS, knowing 9 biomarkers are considered drivers for mutation, but then we’re doing it again. We’re doing a whole next-generation panel. We’re doing both for the advanced metastatic patient, both tissue and liquid with the third party to ensure that we don’t miss a possible mutation because of the heterogeneity of the tumor within lung cancer. Recently there has been approval in the adjuvant setting, which changed the ball game as well. So it’s not so much just in the advanced stage or the metastatic patient’s journey they may need to see medical oncology in that resectable stage, that 1B to 3A, and meet with an oncologist to test for EGFR mutation. That’s how their journey starts. Dr Levy and Dr Scott are great in terms of giving an overview. But we all know as APs and as nurses patients will still reach out with questions in regards to what this means. Why are we waiting for treatment, especially in the metastatic space? When do we start therapy? What do the biomarkers mean? So it’s important for a registered nurse to understand what these biomarkers mean and how they will affect the treatment options the oncologist will discuss with them.
Benjamin P. Levy, MD: Great overview. As Rasheda mentioned, in lung, it’s both tissue and liquid for every patient. We know that if we add liquid to tissue, we are able to unearth additional alterations that we missed in tissue. Interestingly, at our institution, we cannot have reflexive testing because the pathologist cannot be the ordering physician for NGS at our institution. So we have to have either an order set on Epic or an email. It has slowed things down. But we’re really wrestling with this given how important it is for us and all the disciplines to understand what’s going on to make these treatment decisions. Liquid has been our savior in a lot of ways because we can get that turnaround time in 5 days when tissue takes forever and much of it is exhausted and burnt.
Transcript is AI-generated and edited for clarity and readability.
Related Content: